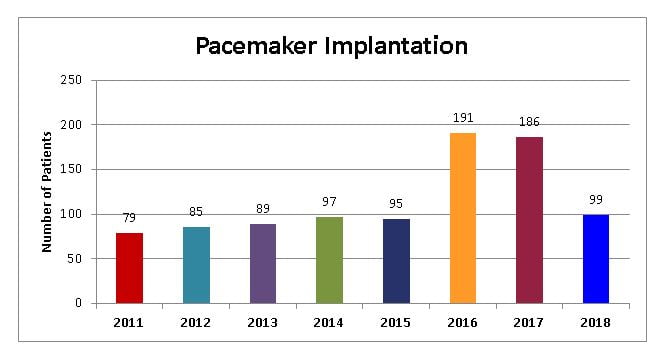
Pacemaker Implantation
An artificial pacemaker is a device that helps the heart muscle pump, or contract, properly. It is operated by a battery. Some pacemakers are placed permanently under the skin in the chest. Others are temporary and placed over the skin. Wires connect from the pacemaker to the heart. One set of wires sends information to the pacemaker about the contraction rate of the heart. Another set of wires sends signals to the heart to contract if the rate is too slow or if it is missing beats.
You may need an artificial pacemaker if your body’s natural pacemaker is not sending proper signals to the heart muscle. Special heart cells, called pacemaker cells, send electrical signals that cause the heart muscle to contract. With each contraction, blood is squeezed from the heart to the body and the lungs. The heart normally contracts (beats) about 50 to 100 times each minute. The rate of beating increases or decreases in response to your activities.Sometimes a heart attack, infection, medicine, or disease damages the heart. As a result, the pacemaker cells may not work properly. When they do not send signals correctly, your heart rate may be fast, irregular, or slow. You may feel like your heart is beating harder or faster. It may feel like it is skipping beats. When your heart beats too fast or too slowly, it may not pump enough blood for your body’s needs. You may feel lightheaded, tired, or faint.
The pacemaker battery usually lasts 4 to 12 years. Your health care provider will be alerted to the fact that it is time to replace the battery during follow-up exams. He or she will check your pacemaker using a small table-top computer, called a programmer, and a wand. The wand is about the same size as a remote control. Your provider puts the wand on your body, about where the pacemaker is located. This allows your health care provider to get information from the pacemaker about how well your heart is working and to check the battery. It is not painful, and it usually takes just a few minutes. You will have plenty of time before the battery is fully used up to plan for replacement. When a battery needs to be replaced, the whole pacemaker will be replaced. Most often, this procedure is very simple. Your health care provider reopens the pocket holding the pacemaker and disconnects the old device from its leads. He or she attaches a new pacemaker to the existing leads, and sews the pocket closed.
A pacemaker allows people with irregular heartbeats to lead normal lives. Pacemakers have been successfully implanted since the early 1950’s. Millions of people have benefited from their use.
When you have a pacemaker, you need to be aware of your surroundings and the devices that may interfere with pacemakers: X-rays generally appear to have no effect on pacemakers, but radiation used to treat cancer may damage the circuits of the pacemaker.
Tell all your health care providers and dentists that you have a pacemaker. Be sure to carry an ID card with you that says you have a pacemaker.
Some people who need a permanent cardiac pacemaker to control their heart rhythm find that they feel worse after the pacemaker is in place. Although they no longer have fainting spells, they feel tired and listless. They notice pounding in the neck or chest, and generally don’t perform activities as well as they once did. This is called pacemaker syndrome, and it sometimes make them wonder whether the procedure was worth the result.
Why does it occur?
The heart’s pumping action depends on a number of things. It needs good inflow from the veins, a proper rate of beating, and heart muscle that squeezes well. The heart also needs to squeeze in a proper pattern. Each heartbeat starts with squeezing (contraction) of the upper heart chambers (atria). A short pause is then followed by contraction of the lower heart chambers (ventricles). If the pattern is changed even slightly, the heart doesn’t pump efficiently.
Pacemaker patients help make the diagnosis by telling their doctor about their symptoms. An electrocardiogram (a painless procedure that records the heart’s electrical activity) or a 24-hour tape recording of the electrocardiogram may be needed to identify just what’s happening. The doctor may find abnormal pulsations in the veins of the neck at the physical exam.
Modern pacemakers can be programmed to change their pattern. The doctor may change heart rates, strength of impulse, and the small built-in pauses that are part of heart contraction. Most of the symptoms can be made better by changing these settings. Several tries with different settings may be necessary. On rare occasions, the pacemaker may need to be replaced by one that can pace both the atria and ventricles, or by a pacemaker that can respond to exercise by increasing its beating rate.
With the right pacemaker and the right adjustments almost all pacemaker syndromes disappear.
Pacemaker Implantation
Pacemaker implantation is a procedure in which the health care provider places a pacemaker in your chest.
This procedure is most often done when your heart rate is too slow. As a result of the abnormal rate, your heart pumps less blood, causing symptoms such as fatigue, shortness of breath, or fainting.
Plan for your care and recovery after the operation, especially if you are to have general anesthesia. Allow for time to rest and try to find people to help you with your day-to-day duties.
Follow any instructions your health care provider may give you. If you are to have general anesthesia, eat a light meal, such as soup or salad the night before the procedure. Do not eat or drink anything after midnight and the morning before the procedure. Do not even drink coffee, tea, or water.
No special preparation is needed for local anesthesia.
You will be given a general or local anesthetic. A general anesthetic will relax your muscles and make you feel as if you are in a deep sleep. It will prevent you from feeling pain during the operation. A local anesthetic, usually combined with mild sedatives, also will keep you away from feeling pain during the operation. If you feel discomfort during the procedure, tell your health care provider immediately.
What happens after the procedure?
- You may stay in the hospital for 1 to 3 days, depending on your condition. You will remain in bed and your heart will be monitored. The day after the procedure you will be encouraged to walk in preparation for leaving the hospital.
- Before you leave the hospital, your health care provider will check your pacemaker using a small table-top computer, called a programmer, and a wand. The wand is about the same size as a remote control. Your provider puts the wand on your body, about where the pacemaker is located. This allows your health care provider to get information from the pacemaker about what the heart is doing and how well it is working. If needed, your health care provider can adjust the pacemaker using the programmer and the wand. It is not painful, and it usually takes just a few minutes.
- You may learn how to check the function of the pacemaker using the telephone. The function of the pacemaker can also be checked at follow-up visits with your health care provider.
- Your health care provider may explain how having a pacemaker might affect your lifestyle and when the battery in the pacemaker may need to be replaced.
- Ask your health care provider what other steps you should take and when you should come back for a checkup.
What are the benefits of this procedure
- Your heart may beat in a healthy rhythm, and you may resume a more normal lifestyle.
- What are the risks associated with this procedure?
- There are some risks when you have general anesthesia. Discuss these risks with your health care provider.
- Local anesthesia may not numb the area quite enough and you may feel some minor discomfort. Also, in rare cases, you may have an allergic reaction to the drug used in this type of anesthesia. Local anesthesia is considered safer than general anesthesia.
- The wire could puncture one of the lungs, the vein, or the heart cavity.
- The pacemaker is implanted because the heart rhythm is abnormal. This may be associated with other heart problems, which could worsen despite correction of the rhythm.
- Like any electrical/mechanical device, the pacemaker may need a replacement if it stops working properly. The pacemaker wire may become dislodged and/or break.
- There is a risk of infection and/or bleeding. You should ask your health care provider how these risks apply to you.
When should I call the health care provider?Call the health care provider immediately if your pulse becomes abnormally slow, fast, or irregular, or your original symptoms return. Call the health care provider during office hours if:
- You have questions about the procedure or its result.
- You want to make another appointment.