Overview
Hypotension is the medical term for low blood pressure (less than 90/60).
A blood pressure reading appears as two numbers. The first and higher of the two is a measure of systolic pressure, or the pressure in the arteries when the heart beats and fills them with blood. The second number measures diastolic pressure, or the pressure in the arteries when the heart rests between beats. 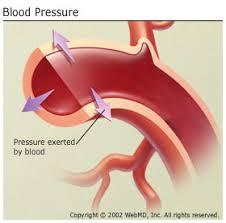
Optimum blood pressure (systolic / diastolic) is below 120/80. Low blood pressure is typically not a problem in healthy people without signs and requires no care. However, low blood pressure may indicate an underlying problem, particularly in the elderly, in which the heart, brain and other vital organs are affected by inadequate blood flow.
Chronic low blood pressure that have no signs are not serious. But health problems can occur when blood pressure suddenly drops and the brain’s blood supply is insufficient. Dizziness or lightheadedness can result. The most common occurrence of sudden drops in blood pressure occurs when someone lying down or sitting down, tries to stand. The low blood pressure is referred to as postural or orthostatic hypotension. When anyone stands for a long period of time, another form of low blood pressure can occur. It is known as neurally mediated hypotension. If it leads to falling down, it is called a vasovagal syncope.
A cardiovascular system or nervous system fails to react adequately to sudden changes is considered to be postural hypotension. Usually, when you wake up, the blood pools in lower extremities If this is not corrected, your blood pressure will fall. But Normally, your body compansate by sending messages to your heart to beat faster and to constrict blood vessels. The drop in blood pressure is compensated by this. If this does not or occur too slowly, the result of postural hypotension may lead to fainting. The risk of both low and high blood pressure normally increases with age due to changes occuring during aging. In addition, blood flow to the heart muscle and the brain declines with age, often as a result of plaque buildup in blood vessels. An estimated 10% to 20% of people over age 65 have postural hypotension.

Causes
It’s not always clear what causes low blood pressure. The following may be linked:
- Pregnancy
- Hormonal disorders like hypothyroidism, diabetes or low blood glucose (hypoglycemia) Hormone disorder
- Some over-the-counter medications
- Some prescription medicines such as medicines for high blood pressure, depression or Parkinson’s disease
- Heart failure
- Heart arrhythmias (abnormal heart rhythms)
- Widening, or dilation, of the blood vessels
- Liver disease
Symptoms
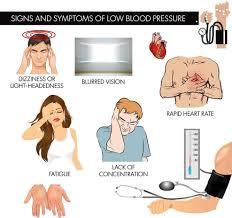
- Dimming or blurring of vision
- Dizziness
- Lightheadedness
- Unsteadiness
- Rapid heart rate
- Weakness and Fatigue
- Nausea
- Pale extrimities
- Lack of concentration
Diagnosis
The doctor will look at your medical history, your age, your specific illness symptoms and your conditions. He or she can do a physical examination and will monitor your blood pressure and pulsation regularly — after a couple of minutes lying down, just after you get up, and after a few minutes you get still.
Many measures such as ECG (electrocardiogram) can be performed to assess the rhythm of the heart rate and pulse and an Echocardiogram to know about Structural heart disease . You should also conduct blood tests to see for anemia or blood sugar problems.
Sometimes, home ECG monitoring (a Holter monitor or an event monitor) may be used to check for an abnormal and or Irregular pulse which could unexpectedly cause the blood pressure to drop.
A Exercise stress test (TMT test) may also help. Less often, an electrophysiological test (EP Test) may be done.
Some forms of postural hypotension may require a test called a “tilt table” test. This test assesses the body’s response to position changes. The person is lying on a table and locked up securely for up to an hour. The table is raised. The blood pressure, heart rate and other symptoms are noted. Medicines are often administered to guide treatment.
Treatment
Many people can effectively treat chronic low blood pressure through diet and changes in lifestyle.
- Eat a diet higher in salt.
- Drink lots of nonalcoholic fluids.
- Limit alcoholic beverages.
- Drink more fluids during hot weather and while sick with a viral illness, such as a cold or the flu.
- Have your doctor evaluate your prescription and over-the-counter medications to see if any of them are causing your symptoms.
- Get regular exercise to promote blood flow.
- Take care when you rise from sitting or lying down. Pump your feet and ankles before you stand up a few times to help improve circulation. Then slowly go ahead. Just a few minutes before you come out of bed, sit up on the edge of the bed.
- If the problem persists even after doing all these measures, you may require the medications. The following medications are often used to treat low blood pressure.
Fludrocortisone. Fludrocortisone is a medication that seems to help most types of low blood pressure. It works by promoting sodium retention by the kidney, causing fluid retention and some bloating, which is necessary to improve blood pressure. But this sodium retention also causes a loss of potassium. So when taking fludrocortisone it is important to get enough potassium every day. Fludrocortisone does not have any of the anti-inflammatory properties of cortisone or prednisone and does not build muscle like anabolic steroids.
Midodrine. It is used to help increase standing blood pressure in people with postural hypotension related to nervous system dysfunction.

