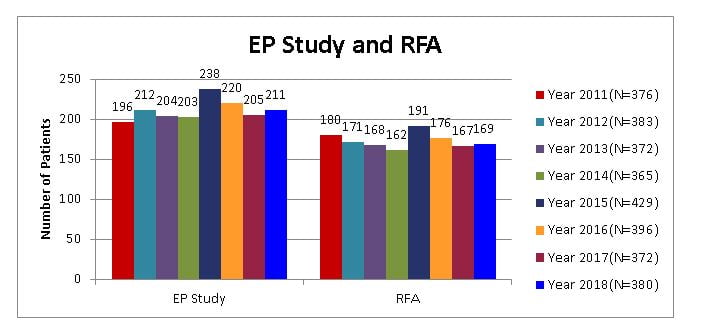
Electrophysiology Studies And RF Ablations
Electrophysiology studies (EPS) for diagnosis of cardiac arrhythmias.
Radio frequency ablation (RFA) of complex cardiac arrhythmias.
Pacemaker therapy (single, dual chamber and multi-site pacing).
Implantable Cardioverter Defibrillator (ICD) for ventricular arrhythmias.
Biventricular pacing therapy for heart failure.
Tilt Table Test for diagnosis in pre-syncope and syncope.
Holter study (24 hour EKG monitoring) for evaluation of symptoms.
Treadmill test (TMT) for inducibility of arrhythmias’ during exercise.
Non-invasive EP testing (NIPS) for evaluation of ICD function.
Clinical management of complex cardiac arrhythmias.
What are arrhythmias and which patients should be suspected of having them?
Arrhythmias are abnormal rhythms of the heart and can be life-threatening.
Patients with Palpitations (uncomfortable awareness of heart beats, rapid heart beats), Pre-syncope (giddiness, feeling faint), and Syncope (fainting, unexplained falls, and spells of unconsciousness) may have cardiac arrhythmias.
What is done during Electrophysiology study (EPS)?
Special electrode catheters (long flexible wires) are introduced through sheaths in the groin into different chambers of the heart and electrical signals are recorded from different sites and displayed on the computerized EP system.
Electrical impulses are delivered from the EP system through the catheters to the heart to stimulate it and induce arrhythmias. Thereafter, various maneuvers are performed and the abnormal focus or pathway is localized.
What is Radiofrequency Ablation (RFA)?
The EPS is performed to diagnose the problem, whereas RFA is, done to treat it. In most cases, it is just continuation of the EPS and performed at the same sitting.
After localizing the abnormal focus or pathway, radiofrequency energy is passed through the catheter to heat up the catheter tip and destroy the abnormal tissue that causes the arrhythmia. This permanently cures the arrhythmia.
What are the benefits of EPS and RFA?
RFA provides permanent cure for the arrhythmia.
A firm diagnosis is achieved for the patient’s symptoms and abnormal EKGs.
In most cases, it avoids a lifetime of medications or anti arrhythmic drugs.
The patient can lead a normal life, free from the psychological stress of impending palpitations.
In cases where absolute cure is not possible (such as chronic Atrial fibrillation or Multiple morphologies of VT), the severity and frequency of chronic arrhythmias can be reduced, which makes their management easier.
Which arrhythmias can be treated with EPS and RFA?
Supraventricular arrhythmias such as A VNRT, A VRT due to WPW syndrome or
concealed accessory pathways, Ectopic atrial tachycardia, atrial flutter, paroxysmal focal atrial fibrillation.
Idiopathic ventricular tachycardias such as RVOT tachycardia, Fascicular tachycardias, Bundle-branch reentrant tachycardias, some cases of ischemic VT.
In certain arrhythmias where absolute cure is not possible, EPS and RFA can be utilized to decrease the burden of arrhythmias which make their management casicr.
Some arrhythmias can be managed with hybrid therapy of RFA combined with device therapy.
What is the success rate?
The success rate depends on the type of arrhythmia and is > 95% in most supraventricular reentrant tachycardias. In ventricular arrhythmias of idiopathic nature, the success rate is 80 – 90%. In recurrent ischemic VT, the success rate is 50 – 70% and requires specialized mapping techniques.
What is the recurrence rate?
After successful ablation, the recurrence rate in supraventricular arrhythmias is less than 5 %. Usually, the recurrences are of benign nature and can be easily managed with a small dose of medications. In most of these cases, re-ablation can be performed successfully.
In ventricular arrhythmias, the recurrence rate is 10 – 15 % (depending on type of arrhythmia). Usually, these VTs can be easily managed with small dose of medications. In some cases, re-ablation may be performed.
Is EPS and RFA safe?
EPS and RFA -are “invasive” procedures requiring insertion of catheters in the body. Thus there is smile risk involved, however this risk is small .
In rare cases (less than 1 in 500), the normal electrical system of the heart may get damaged, which may necessitate insertion of an artificial pacemaker.
In rare cases (less than 1 in 500), hemo-pericardium can occur which is promptly treated with Pericardiocentesis.
Occasional cases may have local vascular problems (such as hematoma) at the groins at site of skin pl1l1cture for catheter insertion.