Atherosclerosis

Introduction
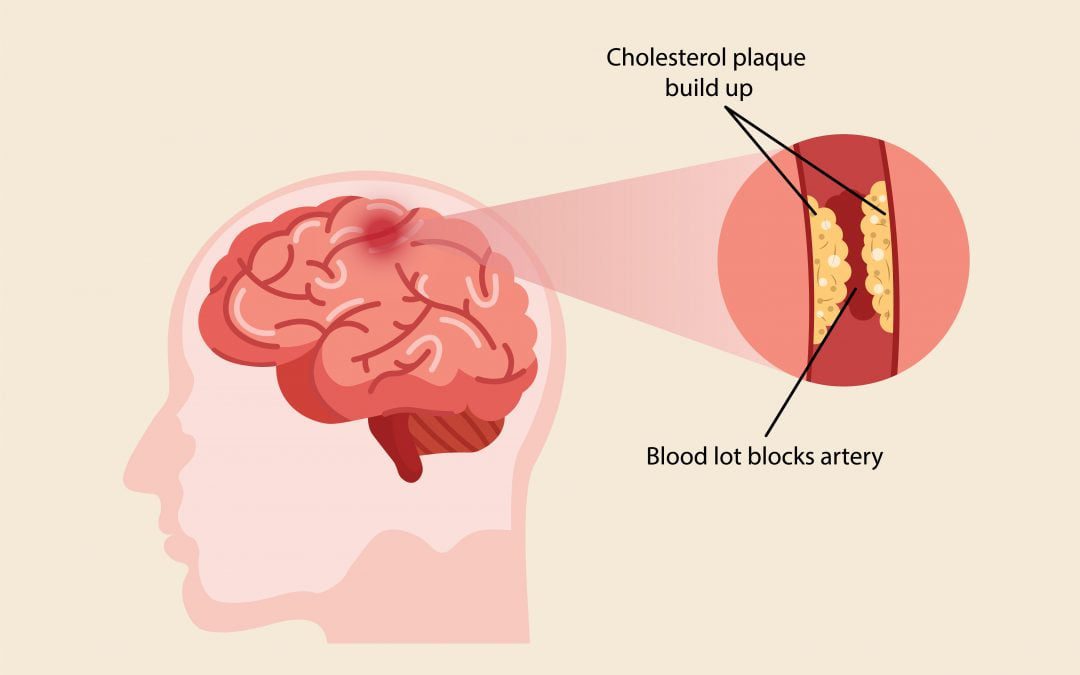
Hardening of the arteries, also called atherosclerosis, is a common disorder. It occurs when fat, cholesterol, and other substances build up in the walls of arteries and form hard structures called plaques. Over time, these plaques can block the arteries and cause symptoms and problems throughout the body.
Causes
Over the course of years and decades, plaque buildup narrows arteries and makes them stiffer. These changes make it harder for blood to flow through them. Clots may form in these narrowed arteries and block blood flow. Pieces of plaque can also break off and move to smaller blood vessels, blocking them. Either way, the blockage starves tissues of blood and oxygen, which can result in damage or tissue death (necrosis). This is a common cause of heart attack and stroke. If a clot moves into an artery in the lungs, it can cause a condition known as pulmonary embolism. In some cases, the plaque is part of a process that causes a weakening of the wall of an artery.
This can lead to an aneurysm. Aneurysms can break open (rupture), and cause bleeding that can be life threatening. Hardening of the arteries is a process that often occurs with aging. However, high blood cholesterol levels can make this process happen at a younger age. For most people, high cholesterol levels are the result of an unhealthy lifestyle — most commonly, eating a diet that is high in fat. Other lifestyle factors are heavy alcohol use, lack of exercise, and being overweight. Other risk factors for hardening of the arteries are diabetes, family history of hardening of the arteries, high blood pressure and smoking.
Symptoms
Atherosclerosis usually doesn’t cause signs and symptoms until it severely narrows or totally blocks an artery. Many people don’t know they have the disease until they have a medical emergency, such as a heart attack or stroke. Some people may have signs and symptoms of the disease. Signs and symptoms will depend on which arteries are affected. The coronary arteries
supply oxygen-rich blood to heart. If plaque narrows or blocks these arteries (a disease called coronary heart disease, or CHD), a common symptom is angina. Angina is chest pain or discomfort that occurs when heart muscle doesn’t get enough oxygen-rich blood. Angina may feel like pressure or squeezing in chest. The patient also may feel it in his shoulders, arms, neck, jaw, or back. Angina pain may even feel like indigestion.
The pain tends to get worse with activity and go away with rest. Emotional stress also can trigger the pain. Hardening of the arteries does not cause symptoms until blood flow to part of the body becomes slowed or blocked. If the arteries to the heart become narrow, blood flow to the heart can slow down or stop. This can cause chest pain (stable angina), shortness of breath, and other symptoms. Narrowed or blocked arteries may also cause problems and symptoms of the intestines, kidneys, legs, and brain. Other symptoms of CHD are shortness of breath and arrhythmias. Arrhythmias are problems with the rate or rhythm of the heartbeat. Plaque also can
form in the heart’s smallest arteries and cause angina, shortness of breath, sleep problems, fatigue (tiredness), and lack of energy.
Major Risk Factors
The exact cause of atherosclerosis isn’t known. However, certain traits, conditions, or habits may raise risk for the disease. These conditions are known as risk factors. The more risk factors the patient has, the more likely it is that he will develop atherosclerosis. The patient can control most risk factors and help prevent or delay atherosclerosis. Other risk factors can’t be controlled. Major risk factors include:

Unhealthy Blood Cholesterol Levels: This includes high LDL cholesterol (also called “bad” cholesterol) and low HDL cholesterol (also called “good” cholesterol). LDL has chemical properties that can damage arteries. Damaged areas allow more LDL to penetrate artery walls. The LDL gets stuck and accumulates in the artery’s wall which leads to atherosclerosis.

High Blood Pressure: Blood pressure is considered high if it stays at or above 140/90 mmHg over time. If the patient has diabetes or chronic kidney disease, high blood pressure is defined as 130/80 mmHg or higher. (The mmHg is millimeters of mercury—the units used to measure blood pressure.) People with high blood pressure are more likely to develop coronary artery disease, because high blood pressure puts added force against the artery walls. The narrowed artery limits or blocks the flow of blood to the heart muscle, depriving the heart of oxygen. Over time, this extra pressure can damage the arteries, making them more vulnerable to the narrowing and plaque buildup associated with atherosclerosis.

Smoking: Smoking can damage and tighten blood vessels, raise cholesterol levels, and raise blood pressure. Smoking also doesn’t allow enough oxygen to reach the body’s tissues. The toxins in tobacco smoke lower a person’s HDL while raising levels of LDL which damage’s heart arteries. Nicotine and Carbon Monoxide in cigarette smoke damage the endothelium, which
sets the stage for the build-up of plaque which ultimately leads to atherosclerosis.

Insulin Resistance & Diabetes: This condition occurs if the body can’t use its insulin properly. Insulin is a hormone that helps move blood sugar into cells where it’s used as an energy source. Insulin resistance may lead to diabetes. With diabetes, the body’s blood sugar level goes high because the body doesn’t make enough insulin or doesn’t use its insulin properly. When too much cholesterol accumulates in arteries with fatty deposits called plaques, due to high blood sugar level, atherosclerosis, or hardening of the arteries occurs.

Overweight or Obesity: The terms “overweight” and “obesity” refer to body weight that’s greater than what is considered healthy for a certain height. Being overweight or obese does not directly increase the risk of developing atherosclerosis and cardiovascular disease (CVD), but it
does lead to related risk factors that do. In particular, overweight or obese people have an increased risk of developing high blood pressure, tend to have higher levels of cholesterol as a result of eating a high-fat diet and have an increased risk of developing type 2 diabetes. Therefore, ultimately obesity leads to atherosclerosis because of its risk factors.

Lack of Physical Activity: A lack of physical activity can worsen other risk factors including high blood pressure, obesity, high cholesterol, and diabetes which eventually lead to atherosclerosis.

Unhealthy diet: An unhealthy diet can raise risk for atherosclerosis. People who frequently take foods that are high in saturated and trans fats, cholesterol, sodium (salt), and sugar can develop obesity, high blood pressure and diabetes. All these ultimately lead to atherosclerosis.

Older age: As the patient gets older, his risk for atherosclerosis increases. Genetic or lifestyle factors cause plaque to build up in arteries as the patient ages. By the time the patient becomes middle-aged or older, enough plaque has built up to cause signs or symptoms. In men, the risk increases after age 45. In women, the risk increases after age 55.

Family history of early heart disease: The risk for atherosclerosis increases if the patient’s father or a brother was diagnosed with heart disease before 55 years of age, or if mother or a sister was diagnosed with heart disease before 65 years of age. Although age and a family history
of early heart disease are risk factors, it doesn’t mean that the patient will develop atherosclerosis if he has one or both. Controlling other risk factors often can lessen genetic influences and prevent atherosclerosis, even in older adults.

Sleep apnea: Sleep apnea is a disorder that causes one or more pauses in breathing or shallow breaths while the patient sleeps. Untreated sleep apnea can raise risk for high blood pressure, diabetes (both diseases lead to atherosclerosis) and even a heart attack or stroke.

Stress: Research shows that the most commonly reported “trigger” for a heart attack is an emotionally upsetting event, especially the one which involves anger. Because of today’s fast life and workload, lot of people live stressful life, which leads to hypertension which is of risk factors of atherosclerosis.

Alcohol: Heavy drinking can damage the heart muscle and worsen other risk factors for atherosclerosis. Drinking an excessive amount of alcohol can cause high blood pressure (hypertension) and raised blood cholesterol levels, increasing the risk of developing atherosclerosis and cardiovascular diseases.
Diagnosis
The doctor may recommend one or more tests to diagnose atherosclerosis. These tests also can help doctor learn the extent of disease and plan the best treatment.
Physical Exam
During the physical exam, the doctor may listen to arteries for an abnormal whooshing sound called a bruit. The doctor can hear a bruit when placing a stethoscope over an affected artery. A bruit may indicate poor blood flow due to plaque buildup. The doctor also may check to see whether any of pulses (for example, in the leg or foot) are weak or absent. A weak or absent
pulse can be a sign of a blocked artery.
Blood Tests
Blood tests check the levels of certain fats, cholesterol, sugar, and proteins in blood. Abnormal levels may be a sign that the patient is at risk for atherosclerosis.
EKG (Electrocardiogram)
An EKG is a simple, painless test that detects and records the heart’s electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through the heart. An EKG can show signs of heart damage caused by CHD. The test also can show signs of a previous or current heart attack.
Chest X Ray
A chest x ray takes pictures of the organs and structures inside chest, such as heart, lungs, and blood vessels. A chest x ray can reveal signs of heart failure.
Ankle/Brachial Index
This test compares the blood pressure in ankle with the blood pressure in arm to see how well blood is flowing.
Echocardiography
Echocardiography (echo) uses sound waves to create a moving picture of heart. The test provides information about the size and shape of heart and how well heart chambers and valves are working. Echo also can identify areas of poor blood flow to the heart, areas of heart muscle that aren’t contracting normally, and previous injury to the heart muscle caused by poor blood flow.
Computed Tomography Scan
A computed tomography (CT) scan creates computer-generated pictures of the heart, brain, or other areas of the body. The test can show hardening and narrowing of large arteries. A cardiac CT scan also can show whether calcium has built up in the walls of the coronary (heart) arteries. This may be an early sign of CHD.
Stress Testing
During stress testing, the patient exercises to make his heart work hard and beat fast while heart tests are done. If the patient can’t exercise, he may be given medicine to make his heart work hard and beat fast. When the heart is working hard, it needs more blood and oxygen. Plaquenarrowed arteries can’t supply enough oxygen-rich blood to meet heart’s needs. A stress test can show possible signs and symptoms of CHD, such as abnormal changes in heart rate or blood pressure, shortness of breath or chest pain, and abnormal changes in heart rhythm or heart’s electrical activity. As part of some stress tests, pictures are taken of the heart while the patient exercises and while he rests. These imaging stress tests can show how well blood is flowing in various parts of heart. They also can show how well the heart pumps blood when it beats.
Angiography
Angiography is a test that uses dye and special x rays to show the inside of arteries. This test can show whether plaque is blocking arteries and how severe the blockage is. A thin, flexible tube called a catheter is put into a blood vessel in his arm, groin (upper thigh), or neck. Dye that can
be seen on an x-ray picture is injected through the catheter into the arteries. By looking at the xray picture, the doctor can see the flow of blood through arteries.
Treatment
To help prevent hardening of the arteries, the patient should make various lifestyle changes. He should avoid fatty foods and eat well-balanced meals that are low in fat and cholesterol. He should include several daily servings of fruits and vegetables and add fish to his diet at least twice a week may be helpful. However, he should not eat fried fish. He should limit alcohol he
drinks probably one drink a day for women, two a day for men. He should exercise for 30 minutes a day if he is not overweight, and for 60 – 90 minutes a day if he is overweight. He should quit smoking which is the single most important change the patient can make to reduce his risk of heart disease and stroke. The patient should get his blood pressure checked every 1 – 2 years before age 50 and yearly after age 50. He should get his blood pressure checked more often if he has high blood pressure, heart disease, or he have had a stroke.
He should consult his doctor about how often he should have his blood pressure checked. If his blood pressure is high, it is important for him to lower it and keep it under control. Everyone should keep their blood pressure below 140/90 mmHg. If the patient has diabetes, kidney disease, or have had a stroke or heart attack, his blood pressure should probably be less than 130/80 mm/Hg. He should check with his doctor about his normal blood pressure range. The doctor may prescribe him medicine for high cholesterol levels if lifestyle changes do not work. This will depend on patient age, whether he has heart disease or other blood flow problems,
whether he smokes or is overweight and if he has high blood pressure or diabetes. The doctor may suggest taking aspirin or another drug called clopidogrel (Plavix) to help prevent blood clots from forming in arteries. These medicines are called antiplatelet drugs. The patient should not
take aspirin without first talking to his doctor.
Outlook (Prognosis)
Hardening of the arteries cannot be reversed or turned back once it has occurred. However, lifestyle changes and treating high cholesterol levels can prevent or slow the process from becoming worse.
Possible Complications
Abdominal aortic aneurysm, coronary artery disease, kidney disease, mesenteric artery ischemia, peripheral artery disease, renal artery stenosis and stroke.
Alternative Names
Hardening of arteries, arteriosclerosis, plaque buildup – arteries